Experience In Rheumatology : 10+ years
- DM (Doctorate of Medicine) in Rheumatology from the King George's Medical University
- Speciality Certificate (Rheumatology) from Royal College of Physicians, UK (MRCP,UK)
- MD (Doctor of Medicine) in General Medicine from Safdarjung Hospital, New Delhi, India
Achievements
- Secured first rank (Gold Medal) at Safdarjung Hospital & Vardhman Mahavir Medical College for the degree of MD (Medicine), for the session 2009-2012.
- Gold Medal (Endowment Prize) in Surgery during MBBS, 2006
- Gold Medal (Endowment Prize) in Ophthalmology during MBBS, 2005.
- 2001: All India Senior School Certificate Examination (AISSCE) (CBSE), CRPF Public School, Rohini, Delhi (88%)
Our Specifications

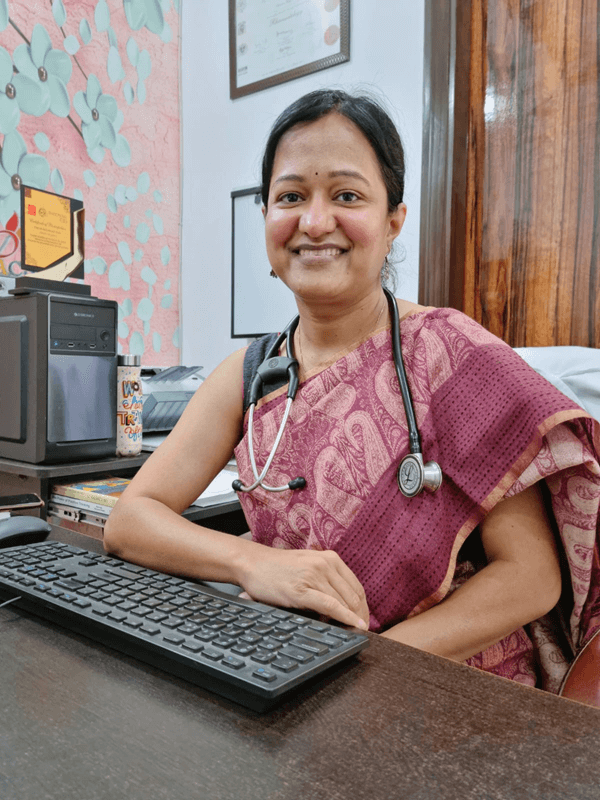
Dr. Meha Sharma is a distinguished Rheumatologist both for adults as well as children (pediatric age group).
Dr. Meha is on the forefront among the new generation of rheumatologists from India, who believe in newer innovations in the practice of rheumatology with the aim of improving patient care, comfort and satisfaction. She has contributed several important original research papers in the field of rheumatology.
She bring with him more than 8 years of experience in Rheumatology; and more than 15 years of experience in Medicine. She has a strong belief in medical ethics and believes in promoting honest ethical clinical practices.
She was previously associated with the prestigious King George’s Medical University Lucknow (2013-2016).
- Consultant And Head, Department Of Rheumatology, Venkateshwar Hospitals, Dwarka, New Delhi
- Member, Academic Committee, Venkateshwar Hospitals, Dwarka, New Delhi
- Member, Women Welfare Committee, Venkateshwar Hospitals, Dwarka, New Delhi
Frequently Asked Questions
Can’t find answer? Mail us at cedarcliniclabs@gmail.com call +91 9911544096
Arthritis affects 15% people i.e. over 180 million people in India. This prevalence is higher than many well known diseases such as diabetes, AIDS and cancer. Rheumatology is a holistic super specialty of Internal Medicine that deals with arthritis and rheumatism. Rheumatism indicates pain arising from joints or other elements of musculoskeletal system. There are over 100 rheumatological disorders classified by World Health Organization. Shortage of trained rheumatologists in India has led to management of these diseases by untrained doctors, practitioners of alternative medicine and quacks. Insufficient appreciation of rheumatological problems appears to be due to lack of knowledge about these conditions. arthritis-india aims at providing scientific information on arthritis and allied conditions and help patients overcome their problems.
All patients with joint and back pain, especially if associated with swelling and stiffness in morning or after a period of rest, must see a rheumatologist at an earliest possible date. Delay in reaching specialist Rheumatology services is the most frequent cause of irreversible joint damage. A rheumatologist can save cost of therapy by avoiding unnecessary investigations and by reducing loss of work-days with proper diagnosis and effective management. The domain of Rheumatology also includes bone, muscle and systemic diseases such as osteoporosis, myositis, systemic lupus and vasculitis. Any patient with unexplained fever, anemia, weakness, weight loss, fatigue, loss of appetite and recurrent abortions should also be assessed by a Rheumatologist.
Joints are surrounded by various structures such as muscles, tendons, ligaments and bursae (Bursa = fluid filled sac between bone and tendons meant for easier movements of tendons). Pain in these structures (also known as soft tissue rheumatism) can be confused with pain from within the joint. These conditions are quite common and can be very distressing.Usually caused by overuse, they can interfere with day-to-day activities and adversely affect work performance. Weakness or deformity of a joint strains adjoining structures and can predispose such conditions. Soft tissue rheumatism can thus coexist with joint disease and pose diagnostic problem for general doctors. Soft tissue rheumatism can be easily differentiated from arthritis as the pain in these conditions is superficial and sharply localized. There is a localized area of tenderness (pain on pressure). There will be pain when you move your joint (active movement) but will not occur when someone else moves it (passive movement). Soft tissue rheumatism generally needs adequate rest (an appliance may be needed), training in proper use of affected area and properly guided exercises. Your doctor will prescribe you pain medication (oral drug and ointment for local application) that reduces swelling too. Physiotherapy measures such as ultrasonic heat can be of help in selected cases.
Pain at multiple body areas is a common problem affecting 7-13% of western population. Most studies indicate a female preponderance and association with psychological distress in these cases. Pain is usually present for many years. Generalised pain needs to be distinguished from various forms of arthritis. Pain in these conditions does not have exact localization and usually not restricted to joints. Patients may complain of pain in other areas such as bones, muscles and back. Although severity of chronic generalised or widespread pain can vary from one individual to another it does affect physical functions and emotions leading to diminished quality of life. Chronic widespread pain can occur in children too. These conditions have direct societal impact in addition to direct and indirect medical costs.
Causes of Generalised Pain
Various conditions can cause generalised pain. Some of these are listed below:
1. Flu and many other viral infections including HIV
2. Multiple myeloma and metastatic cancers
3. Neuropathies
4. Depression, anxiety and other psychiatric disorders
5. Anaemia, thyroid and calcium related diseases (Osteomalacia)
6. Rheumatologic disorders - fibromyalgia, myopathies, systemic inflammatory diseases including rheumatoid arthritis
Chronic generalised pain (more than 3 months duration) needs a proper assessment and a few initial investigations. Coexistence with other problems such as fatigue, bowel irregularities and menstrual problem is also known. Widespread pain may be concomitant with diseases mentioned above.
Imagine our body without bones and joints. Bones constitute about 15% of total body weight. Bone is a dynamic structure in a living body. It consists of multiple layers of fibers around which minerals such as calcium are deposited in crystalline form. The hardness and rigidity of bones is due to minerals whereas resilience and toughness is due to fibers. Remodeling of bones (turnover) continues throughout life and is brought about by various bone cells. The remodeling cycle of bone is an orderly process initiated by osteoclasts (cells that destroy bone and form a 'pit') and followed by formation of new bone by cells known as osteoblasts. Bone formation and resorption are in dynamic equilibrium. Calcium is an essential constituent of bones. Vitamin D, formed under the skin on exposure to sunlight, maintains calcium balance and is important in bone formation.
Lofgrens - Psoriasis Lofgrens A58 year old male, a retired bank employee, presented with 3 week history of bilateral ankle pain and swelling. He also had Lofgrens B Lofgrens Hilar Nodesintermittent dry cough that would be continuous on lying down. 2 painless red nodules developed recently on his left lower extremity. He had recent onset fatigue and lost 2 Kg weight during those 3 weeks. He was a known hypertensive on drugs since 10 years and had skin and nail psoriasis since 34 years. Clinical examination revealed synovitis of both ankles and wrists. He had skin and nail psoriasis along with discrete lesions of erythema nodosum on legs and right hand. A few inspiratory crackles could be auscultated on respiratory examination. ESR was 57 mm at one hour, Rheumatoid factor 57 IU and Serum ACE normal. Other laboratory investigations were normal. His X-ray of chest showed hilar prominence confirmed by CT scan to be lymphadenopathy. He was treated with a 4 week tapering course of prednisolone and settled completely without any recurrence for next 3 years. Association with psoriasis appears to be incidental and rarely reported. Sarcoidosis is an inflammatory disorder affecting mainly lungs and lymph nodes. Small inflammatory nodules appear at various sites. It can involve multiple systems including joints, bones, eyes, muscles, liver, spleen and bone marrow. The disease can be mild and asymptomatic to debilitating and lead to death in less than 5% cases. Steroids and methotrexate form mainstay of therapy at present.
A 50 year old army man presented with severe debilitating pain in multiple joints for 6 months along with nodular, itchy skin rashes for 4 months. These were associated with loss of appetite, ulcers in mouth and significant weight loss. Various joints - including small hand joints, wrists, elbows, shoulders, knees and ankles - were swollen, tender, restricted and deformed. There were multiple discrete but grouped reddish brown nodules of varying sizes (2mm-2cm) over lower abdomen, face, forearms, back, buttocks, both knees and ankles. Biopsy of skin lesions confirmed clinical diagnosis of multicentric reticulohistiocytosis. Aggressive therapy with zoledronate and methotrexate was instituted. Pain reduced after a period of 3 months and skin lesions, too, started settling down. At the end of One year, deformities still persist and skin lesions, though milder, keep on cropping up intermittently. Multicentric reticulohistiocytosis is a rare disease with destructive arthritis and skin lesions. The disease can involve other organs and may be associated with underlying malignancy. Exact cause of the disease remains unknown and various drugs seem to offer very limited benefit. The disease can remain active for prolonged period. (8 or more years) often leaving the patient with crippling and deformed joints.
A 23 year old male presented with swelling of both knees. He had history of similar problem 18 months ago treated with joint aspiration and non-steroidal anti-inflammatory drugs. There was no other significant history. Clinical examination revealed another swelling of enthesitis near left ankle. His X-ray revealed osteopoikilosis. Arthritis was treated with non-steroidal anti-inflammatory drugs and settled over a period of 6-8 weeks. Osteopoikilosis is an inherited condition of small, rounded or oval, multiple, symmetric areas of bone sclerosis (increased density) occurring near growing ends and adjacent areas of bones. These densities appear in childhood and persist throughout life. They do not cause any symptoms nor require any treatment.
A 52 year old female complained of intermittent low back pain of varying severity radiating to right thigh since 3 years. The pain was more frequent in cold season and increased after exertion. She underwent hysterectomy 12 years back for dysmenorrhoea. Laboratory investigations, including inflammatory markers, were normal. Her X-ray and MRI showed well defined areas of sclerosis around sacroiliac joints. There was no sacroiliitis. Osteitis condensans ilii is a benign condition more common in obese multiparous females. Low back pain radiating to buttocks is a common feature. Pain is exacerbated by activity and relieved by rest. Back pain may be milder in some cases. X ray shows bilateral symmetric sclerosis on iliac sides of sacroiliac joints. The sclerosis is triangular in shape with base pointing inferiorly. Sacroiliitis needs to be differentiated by clinical examination and MRI in doubtful cases. Similar changes can occur at other sites such as pubic bones and medial end of clavicle. The condition may resolve spontaneously or X-ray picture may change from time to time. Therapy consists of posture correction and active exercises for 6-12 months. A few nonresponsive cases may require sacroiliac fusion surgery.
A 38 year old male had complaints of intermittent pain and mild swelling in ankle and foot joints since 2 years. He was under treatment of a homeopathic doctor without any significant relief. His joint pain was associated with pain in rib cage and sometimes with a change of voice and redness of eyes. He used to feel feverish during these arthritic episodes and was generally unwell, developed loss of appetite and nutritional anaemia. In view of no response to homeopathic drugs, he switched to Ayurveda therapy. The Ayurveda physician prescribed him purging which was followed by severe abdominal pain, diarrhea and dehydration. He was hospitalized for the same where his condition stabilized. He developed pain and mild swelling in some of his joints along with pain in left lower ribs. This was followed by painful, pink, tender and warm swelling of pinna of his left ear – a classic finding in Relapsing Polychondritis. Relapsing Polychondritis is a multisystem autoimmune disease due to swelling of cartilage tissue. Cartilage is a firm (softer than bone) and flexible structure that is found in ear (external as well as internal), nose, glottis (phonating organ in throat), wind-pipe (trachea), rib cage, joints and intervertebral discs. Relapsing Polychondritis can be primary or be associated (30% cases) with various autoimmune and other diseases. Recurrent swelling of ear, nose and other organs leads to deformities (cauliflower ear, saddle nose). Obstruction of wind-pipe, deafness and redness of eye with diminution of vision are dreaded complications occurring in about 50% patients over course of this disease. Defects of heart valves (aortic), swelling of blood vessels, involvement of nervous system and kidneys can also occur in Relapsing Polychondritis. Prognosis of patients with Relapsing Polychondritis has significantly improved in recent years due to better management with drugs and surgery in selected patients.
65 year old Nigerian Indian presented with fever, bone and joint pains as well as severe pain in hands and calf muscles since 3 months. Itchy, extensive skin rash appeared along with. The rash did respond to therapy with residual pigmentation on his forehead. Fever did not respond despite various antibiotics including those used for tuberculosis. He then came to India for further management. His examination revealed pigmentation over forehead, muscle tenderness over extremities, swollen and tender wrist joints and pain and crepitus in both knees (suggestive of osteoarthritis). Blood examination revealed high eosinophil (a type of white blood cell) count and raised ESR. Other laboratory investigations were normal. Fever and myalgia responded to steroids and painkillers. The patient went back to Nigeria after 3 weeks or so. Eosinophilia Myalgia syndrome is closely linked to ingestion of tryptophan in diet although evidence of its ingestion is not essential for diagnosis of this disease. Tryptophan was, therefore, withdrawn from US market in 1991 but sales were again allowed from 2001. Tryptophan is available in food stores as diet supplement. People use it for insomnia, depression and menstrual problems. Average daily dose of 1250 mg for 6 months to 9 years is supposed to lead to this disease. Tryptophan is a routine constituent of most protein-based foods or dietary proteins. Chocolates, oats, bananas, mangoes, dried dates, milk and milk products, spirulina, peanuts, red meat, eggs, fish, poultry and turkey are all rich sources of tryptophan. Symptoms of Eosinophilia Myalgia syndrome can be difficult to respond to therapy. Muscle pain and weakness, fatigue, joint pains, breathlessness, memory loss and numbness can persist even at the end of 1-4 years.
A good history and detailed clinical examination of patient are extremely important for proper diagnosis of over 100 types of arthritis. Recognition of patterns of joint involvement (topography) as well as those of disease presentation and progression is essential for correct clinical diagnosis. In rheumatology practice, a working diagnosis can usually be made on proper examination of the patient. Laboratory tests including X-Rays are ordered later for confirmation of diagnosis, ruling out other possible causes, estimating level of disease activity or monitoring drug toxicity. As with any other investigations, these must be obtained from a reliable laboratory and the results should always be interpreted in view of clinical picture. These tests are costly and must not be used indiscriminately. Laboratory studies are useful in arthritis only if ordered in an appropriate clinical situation and interpreted accordingly. Measurement errors, laboratory variations due to various factors and inherent limitations must always be born in mind. A positive test in absence of appropriate clinical setting can generally be overlooked.
Pain is a universal phenomenon. It is an unpleasant sensation felt by more than half of the world's population. Pain is a perception which is real and leads to considerable deterioration of quality of life in patients with arthritis and other rheumatological conditions. It has complex causes and is a leading cause of morbidity. Pain limits ability to perform day-to-day activities, maintain social relationships and lead productive life. 'Pain is a perfect misery, the worst of evils, and when excessive, overturns all patience' (John Milton). Pain as a sensation starts from sensors in skin and other organs and reaches brain via nerve channels passing through spinal cord. It can be nociceptive (produced by injury), neuropathic (due to irritation of nerve), mixed or psychological. Fast pain is one which occurs after an injury. Localization of this pain is sharp and accurate and is protective in nature. Slow pain is a delayed perception after tissue injury that helps in healing. Descending chemical and electrical impulses from brain modulate pain perception to a significant extent. Pain may be described in various ways such as sharp, shooting, burning, nagging, dull and aching. Being a subjective sensation, it is very difficult to quantify pain. Severity of pain is generally measured by visual analog or numerical rating scales which ask the patients to rate the severity of their pain on a 1-10 or 1-100 scale. Back pain can be as severe as cancer pain whereas severity of arthritis pain can be almost half that of pain during childbirth. Pain leads to restlessness, anxiety and depression. Physical effects of pain include nausea, vomiting, palpitations, urinary incontinence, rise in blood pressure, etc. Pain does need treatment but it must be realized that pain is a protective phenomenon. Pain in arthritis limits movements that can be damaging. Chemical substances released during slow pain help in healing. One must learn to bear and live with at least some of arthritis pain. We have many effective drugs for pain relief, but not all work in patients in identical way. Though invaluable in pain management, they are notorious for causing skin rashes, acidity and other more severe abdominal problems, liver and kidney toxicity as well as effects on heart and blood pressure. They interact with some other drugs such as those used for diabetes and blood pressure. Control of disease causing pain e.g. rheumatoid arthritis alleviates need for pain medication.
Guidelines by European League against Rheumatism (EULAR) on use of pain killers include following:
1. Avoid long term use
2. Use as and when required and not continuously
3. Use lowest effective dose for shortest duration
4. Use only one painkiller at a time
5. Avoid in stomach ulcer and kidney disease.
Prescription of painkillers must be individualized after assessment of need and risk factors. Paracetamol (maximum dose: 4 grams/day) is a comparatively safe painkiller. Local application of heat or ice pack or an ointment should also be tried in all cases of musculoskeletal pain. Patient education regarding self-help, social support, joint protection and assistive devices, physical therapy and exercise, acupuncture and music therapy are important non-drug measures in pain management.
As per World Health Organization (WHO) criteria, your BMI should fall between 18.5 and 24.9 to be normal. If your BMI is between 25 and 29.9 you are overweight. A BMI ≥ 30 classifies you as obese. People who have a BMI of ≥ 40 fall into the ‘morbidly obese’ weight bracket.
Diet and do-don'ts (pathya - suitable versus harmful diet and lifestyle) have gained importance in our country since the period of Ramayan and Mahabharat. Food keeps alive our journey of life hence it is not unnatural for people to think that there is a relation between diet and disease. The importance of pathya is rooted deep in the minds of people over hundreds of years. Scientists all over world are looking for co-relation between diet and arthritis for over last seven decades. Although over half of the arthritis patients are following some or the other pathya, there is no sufficient evidence for some particular diet or dietetic item triggering or flaring or curing arthritis. Magic cure is certainly impossible with the help of diet therapy.
Diet and food supplements are advertised in various books, periodicals and on internet. There is no scientific proof in favor of diet supplements which are usually expensive. Patients fall prey to these advertisements which are usually more expensive than the actual disease modifying drugs. Companies rob these patients by paying hefty commission to their selling agents. Inflammatory arthritis, by its very nature, is a disease of relapse and remissions. Remission in a particular patient on starting with a particular therapy is advertised as success of that particular therapy. Poor people have no knowledge of checking the validity of tall claims in the advertisement.
The list of pathya is sometimes so long that there remains nothing to eat. Some practitioners advise fasting which is not advocated even in Ayurveda. Vagbhata says that insufficient diet reduces strength, nourishment as well as luster and causes all vata-diseases ( Sutra sthan 8/3). Some people advise liquid diet only. These measures may reduce pain to some extent but are not effective in shortening the duration of morning stiffness or controlling the disease or in improving the functional status. Patients start feeling better after 4-5 days of fasting. Fasting can lead to severe fatigue, weakness and weight loss. Switching back to regular diet brings the disease to original status once again. Fasting, liquid diet or other pathya is difficult to maintain indefinitely. Such diets have an overt risk of malnutrition.
It must be understood that arthritis is of more than 100 types which are classified into two major classes-degenerative and inflammatory. It obviously means that the pathya in these two classes of arthritis is not the same because of an altogether different disease process. It is usually advisable to change the diet step by step. One should identify a few dietary items that increase the pain or stiffness. Once identified, such items may be avoided for a month or so. Reappearance of symptoms on reintroduction of suspected item indicates a sort of allergy. Such food items should never ever be consumed again.
Many rheumatologic diseases affect young women of childbearing age. Pregnancy alters immune status and is always a cause of concern in this age group. Effective use of better drugs and rigorous monitoring can now lead to remission of disease activity in many cases. Safe pregnancy and healthy child are thus possible in most cases with controlled disease activity. This issue must be carefully discussed before planning pregnancy in every patient desirous of child bearing. Pregnancy in rheumatic diseases requires a multidisciplinary coordinated approach for best possible outcome.
Pregnancy related issues of some important rheumatologic diseases are listed below:
Rheumatoid Arthritis (RA) : A lower birthrate in patients with RA is possibly due to choices of patients to limit family size rather than effect of the disease on fertility. Disease activity decreases during pregnancy in 75-95% patients. The improvement starts in first trimester and continues till delivery. There is no evidence of fetal growth retardation or increased incidence of abortions. No special monitoring is required during pregnancy. Drugs such as methotrexate and leflunomide must be discontinued 2 and 24 month respectively before planning pregnancy. Pain control during pregnancy with RA should be achieved with safe drugs and non-pharmacologic measures (rest, splints, fomentation, icepack, etc). RA is known to flare up after delivery. New onset of RA following delivery is also common. Use of routine anti-rheumatic drugs is possible after delivery with properly timed breast feeding.
Systemic Lupus Erythematosus (SLE) :Patients with SLE appear to be less fertile due to disease effect (irregular or no menses) or due to effect of drugs (glucocorticoids and cyclophosphamide). Patients on cyclophosphamide are less likely to develop infertility (failure of ovaries) if cyclophosphamide is started at a younger age ( More then 26 years). Ovarian failure is more likely with higher cumulative dose. Concurrent use of Gonadotropin Releasing Hormone reduces the risk of premature ovarian failure. SLE patients are more likely to develop flares during pregnancy (unproven observation) which are usually mild and respond to standard therapy. Patients with inactive disease are less likely to develop flares. Pregnancy, therefore, should be planned during quiescent disease. Risk of intrauterine growth retardation, abortions and stillbirth is generally higher in SLE patients. Antibodies are transmitted to fetus during weeks 16-32 of gestation and can be harmful to fetus. Careful monitoring after week 16 is, therefore, advisable. These antibodies are usually destroyed with first 6 months of life.
Ankylosing spondylitis and other spondyloarthropathies : Pregnancy improves peripheral arthritis and eye problems but worsens back pain. Increase in back pain is possibly due to mechanical causes.
Management of chronic diseases demands informed and active participation of patient. An intelligent and educated patient with some faith in a selected medical specialist is usually better placed for good therapeutic outcome. An intelligent patient can easily analyze own symptoms and express them to doctor. Patients must provide true and correct information to their doctor. Anxious, depressed, forgetful, timid or violent patients with chronic physical disease are usually difficult to treat. Therapy is likely to be unsuccessful in patients who keep on experimenting with dosages of their prescribed drugs. They must follow prescribed treatment religiously and inform new developments correctly. Trust in physician increases chances of adherence to treatment plan. A good doctor-patient relationship can only be built upon trust. Patients must also understand and accept limitations of present therapy in chronically damaged joints and other organs and define expectations accordingly. Finally, adequate resources to fund cost of therapy are absolutely essential.
Washing your hands with soap and water or using alcohol-based hand rub kills viruses that may be on your hands.
When someone coughs or sneezes they spray small liquid droplets from their nose or mouth which may contain virus. If you are too close, you can breathe in the droplets, including the COVID-19 virus if the person coughing has the disease.
Hands touch many surfaces and can pick up viruses. Once contaminated, hands can transfer the virus to your eyes, nose or mouth. From there, the virus can enter your body and can make you sick.
Make sure you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. Then dispose of the used tissue immediately.
The most common symptoms of COVID-19 are fever, tiredness, and dry cough. Some patients may have aches and pains, nasal congestion, runny nose, sore throat or diarrhea. These symptoms are usually mild and begin gradually. Some people become infected but don’t develop any symptoms and don't feel unwell. Most people (about 80%) recover from the disease without needing special treatment. Around 1 out of every 6 people who gets COVID-19 becomes seriously ill and develops difficulty breathing. Older people, and those with underlying medical problems like high blood pressure, heart problems or diabetes, are more likely to develop serious illness. People with fever, cough and difficulty breathing should seek medical attention.
There is no specific medicine to prevent or treat coronavirus disease (COVID-19). People may need supportive care to help them breathe.
If you have mild symptoms, stay at home until you’ve recovered. You can relieve your symptoms if you:
- - Rest and Sleep
- - Weep Warm
- - Drink Plenty of Liquids
- - Use a room humidifier or take a hot shower to help ease a Sore Throat and Cough
If you develop a fever, cough, and have difficulty breathing, promptly seek medical care. Call in advance and tell your health provider of any recent travel or recent contact with travelers.
The following measures ARE NOT effective against COVID-2019 and can be harmful:
- - Smoking
- - Wearing multiple masks
In any case, if you have fever, cough and difficulty breathing seek medical care early to reduce the risk of developing a more severe infection and be sure to share your recent travel history with your health care provider.
Currently, the source of SARS-CoV-2, the coronavirus (CoV) causing COVID-19 is unknown. All available evidence suggests that SARS-CoV-2 has a natural animal origin and is not a constructed virus. SARS-CoV-2 virus most probably has its ecological reservoir in bats. SARS-CoV-2, belongs to a group of genetically related viruses, which also include SARS-CoV and a number of other CoVs isolated from bats populations. MERS-CoV also belongs to this group, but is less closely related.
The virus that causes COVID-19 is mainly transmitted through droplets generated when an infected person coughs, sneezes, or speaks. These droplets are too heavy to hang in the air. They quickly fall on floors or surfaces.
You can be infected by breathing in the virus if you are within 1 metre of a person who has COVID-19, or by touching a contaminated surface and then touching your eyes, nose or mouth before washing your hands.
Arthritis affects 15% people i.e. over 180 million people in India. This prevalence is higher than many well known diseases such as diabetes, AIDS and cancer. Rheumatology is a holistic super specialty of Internal Medicine that deals with arthritis and rheumatism. Rheumatism indicates pain arising from joints or other elements of musculoskeletal system. There are over 100 rheumatological disorders classified by World Health Organization. Shortage of trained rheumatologists in India has led to management of these diseases by untrained doctors, practitioners of alternative medicine and quacks. Insufficient appreciation of rheumatological problems appears to be due to lack of knowledge about these conditions. arthritis-india aims at providing scientific information on arthritis and allied conditions and help patients overcome their problems.
All patients with joint and back pain, especially if associated with swelling and stiffness in morning or after a period of rest, must see a rheumatologist at an earliest possible date. Delay in reaching specialist Rheumatology services is the most frequent cause of irreversible joint damage. A rheumatologist can save cost of therapy by avoiding unnecessary investigations and by reducing loss of work-days with proper diagnosis and effective management. The domain of Rheumatology also includes bone, muscle and systemic diseases such as osteoporosis, myositis, systemic lupus and vasculitis. Any patient with unexplained fever, anemia, weakness, weight loss, fatigue, loss of appetite and recurrent abortions should also be assessed by a Rheumatologist.
Joints are surrounded by various structures such as muscles, tendons, ligaments and bursae (Bursa = fluid filled sac between bone and tendons meant for easier movements of tendons). Pain in these structures (also known as soft tissue rheumatism) can be confused with pain from within the joint. These conditions are quite common and can be very distressing.Usually caused by overuse, they can interfere with day-to-day activities and adversely affect work performance. Weakness or deformity of a joint strains adjoining structures and can predispose such conditions. Soft tissue rheumatism can thus coexist with joint disease and pose diagnostic problem for general doctors. Soft tissue rheumatism can be easily differentiated from arthritis as the pain in these conditions is superficial and sharply localized. There is a localized area of tenderness (pain on pressure). There will be pain when you move your joint (active movement) but will not occur when someone else moves it (passive movement). Soft tissue rheumatism generally needs adequate rest (an appliance may be needed), training in proper use of affected area and properly guided exercises. Your doctor will prescribe you pain medication (oral drug and ointment for local application) that reduces swelling too. Physiotherapy measures such as ultrasonic heat can be of help in selected cases.
Pain at multiple body areas is a common problem affecting 7-13% of western population. Most studies indicate a female preponderance and association with psychological distress in these cases. Pain is usually present for many years. Generalised pain needs to be distinguished from various forms of arthritis. Pain in these conditions does not have exact localization and usually not restricted to joints. Patients may complain of pain in other areas such as bones, muscles and back. Although severity of chronic generalised or widespread pain can vary from one individual to another it does affect physical functions and emotions leading to diminished quality of life. Chronic widespread pain can occur in children too. These conditions have direct societal impact in addition to direct and indirect medical costs.
Causes of Generalised Pain
Various conditions can cause generalised pain. Some of these are listed below:
1. Flu and many other viral infections including HIV
2. Multiple myeloma and metastatic cancers
3. Neuropathies
4. Depression, anxiety and other psychiatric disorders
5. Anaemia, thyroid and calcium related diseases (Osteomalacia)
6. Rheumatologic disorders - fibromyalgia, myopathies, systemic inflammatory diseases including rheumatoid arthritis
Chronic generalised pain (more than 3 months duration) needs a proper assessment and a few initial investigations. Coexistence with other problems such as fatigue, bowel irregularities and menstrual problem is also known. Widespread pain may be concomitant with diseases mentioned above.
Joint Disease
Imagine our body without bones and joints. Bones constitute about 15% of total body weight. Bone is a dynamic structure in a living body. It consists of multiple layers of fibers around which minerals such as calcium are deposited in crystalline form. The hardness and rigidity of bones is due to minerals whereas resilience and toughness is due to fibers. Remodeling of bones (turnover) continues throughout life and is brought about by various bone cells. The remodeling cycle of bone is an orderly process initiated by osteoclasts (cells that destroy bone and form a 'pit') and followed by formation of new bone by cells known as osteoblasts. Bone formation and resorption are in dynamic equilibrium. Calcium is an essential constituent of bones. Vitamin D, formed under the skin on exposure to sunlight, maintains calcium balance and is important in bone formation.
You need to get your blood sugar checked in fasting as well as 2 hours after taking 75gms of glucose. You should consult your doctor for all precautions & information prior to testing.
Lofgrens - Psoriasis Lofgrens A58 year old male, a retired bank employee, presented with 3 week history of bilateral ankle pain and swelling. He also had Lofgrens B Lofgrens Hilar Nodesintermittent dry cough that would be continuous on lying down. 2 painless red nodules developed recently on his left lower extremity. He had recent onset fatigue and lost 2 Kg weight during those 3 weeks. He was a known hypertensive on drugs since 10 years and had skin and nail psoriasis since 34 years. Clinical examination revealed synovitis of both ankles and wrists. He had skin and nail psoriasis along with discrete lesions of erythema nodosum on legs and right hand. A few inspiratory crackles could be auscultated on respiratory examination. ESR was 57 mm at one hour, Rheumatoid factor 57 IU and Serum ACE normal. Other laboratory investigations were normal. His X-ray of chest showed hilar prominence confirmed by CT scan to be lymphadenopathy. He was treated with a 4 week tapering course of prednisolone and settled completely without any recurrence for next 3 years. Association with psoriasis appears to be incidental and rarely reported. Sarcoidosis is an inflammatory disorder affecting mainly lungs and lymph nodes. Small inflammatory nodules appear at various sites. It can involve multiple systems including joints, bones, eyes, muscles, liver, spleen and bone marrow. The disease can be mild and asymptomatic to debilitating and lead to death in less than 5% cases. Steroids and methotrexate form mainstay of therapy at present.
A 50 year old army man presented with severe debilitating pain in multiple joints for 6 months along with nodular, itchy skin rashes for 4 months. These were associated with loss of appetite, ulcers in mouth and significant weight loss. Various joints - including small hand joints, wrists, elbows, shoulders, knees and ankles - were swollen, tender, restricted and deformed. There were multiple discrete but grouped reddish brown nodules of varying sizes (2mm-2cm) over lower abdomen, face, forearms, back, buttocks, both knees and ankles. Biopsy of skin lesions confirmed clinical diagnosis of multicentric reticulohistiocytosis. Aggressive therapy with zoledronate and methotrexate was instituted. Pain reduced after a period of 3 months and skin lesions, too, started settling down. At the end of One year, deformities still persist and skin lesions, though milder, keep on cropping up intermittently. Multicentric reticulohistiocytosis is a rare disease with destructive arthritis and skin lesions. The disease can involve other organs and may be associated with underlying malignancy. Exact cause of the disease remains unknown and various drugs seem to offer very limited benefit. The disease can remain active for prolonged period. (8 or more years) often leaving the patient with crippling and deformed joints.
A 23 year old male presented with swelling of both knees. He had history of similar problem 18 months ago treated with joint aspiration and non-steroidal anti-inflammatory drugs. There was no other significant history. Clinical examination revealed another swelling of enthesitis near left ankle. His X-ray revealed osteopoikilosis. Arthritis was treated with non-steroidal anti-inflammatory drugs and settled over a period of 6-8 weeks. Osteopoikilosis is an inherited condition of small, rounded or oval, multiple, symmetric areas of bone sclerosis (increased density) occurring near growing ends and adjacent areas of bones. These densities appear in childhood and persist throughout life. They do not cause any symptoms nor require any treatment.
A 52 year old female complained of intermittent low back pain of varying severity radiating to right thigh since 3 years. The pain was more frequent in cold season and increased after exertion. She underwent hysterectomy 12 years back for dysmenorrhoea. Laboratory investigations, including inflammatory markers, were normal. Her X-ray and MRI showed well defined areas of sclerosis around sacroiliac joints. There was no sacroiliitis. Osteitis condensans ilii is a benign condition more common in obese multiparous females. Low back pain radiating to buttocks is a common feature. Pain is exacerbated by activity and relieved by rest. Back pain may be milder in some cases. X ray shows bilateral symmetric sclerosis on iliac sides of sacroiliac joints. The sclerosis is triangular in shape with base pointing inferiorly. Sacroiliitis needs to be differentiated by clinical examination and MRI in doubtful cases. Similar changes can occur at other sites such as pubic bones and medial end of clavicle. The condition may resolve spontaneously or X-ray picture may change from time to time. Therapy consists of posture correction and active exercises for 6-12 months. A few nonresponsive cases may require sacroiliac fusion surgery.
A 38 year old male had complaints of intermittent pain and mild swelling in ankle and foot joints since 2 years. He was under treatment of a homeopathic doctor without any significant relief. His joint pain was associated with pain in rib cage and sometimes with a change of voice and redness of eyes. He used to feel feverish during these arthritic episodes and was generally unwell, developed loss of appetite and nutritional anaemia. In view of no response to homeopathic drugs, he switched to Ayurveda therapy. The Ayurveda physician prescribed him purging which was followed by severe abdominal pain, diarrhea and dehydration. He was hospitalized for the same where his condition stabilized. He developed pain and mild swelling in some of his joints along with pain in left lower ribs. This was followed by painful, pink, tender and warm swelling of pinna of his left ear – a classic finding in Relapsing Polychondritis. Relapsing Polychondritis is a multisystem autoimmune disease due to swelling of cartilage tissue. Cartilage is a firm (softer than bone) and flexible structure that is found in ear (external as well as internal), nose, glottis (phonating organ in throat), wind-pipe (trachea), rib cage, joints and intervertebral discs. Relapsing Polychondritis can be primary or be associated (30% cases) with various autoimmune and other diseases. Recurrent swelling of ear, nose and other organs leads to deformities (cauliflower ear, saddle nose). Obstruction of wind-pipe, deafness and redness of eye with diminution of vision are dreaded complications occurring in about 50% patients over course of this disease. Defects of heart valves (aortic), swelling of blood vessels, involvement of nervous system and kidneys can also occur in Relapsing Polychondritis. Prognosis of patients with Relapsing Polychondritis has significantly improved in recent years due to better management with drugs and surgery in selected patients.
65 year old Nigerian Indian presented with fever, bone and joint pains as well as severe pain in hands and calf muscles since 3 months. Itchy, extensive skin rash appeared along with. The rash did respond to therapy with residual pigmentation on his forehead. Fever did not respond despite various antibiotics including those used for tuberculosis. He then came to India for further management. His examination revealed pigmentation over forehead, muscle tenderness over extremities, swollen and tender wrist joints and pain and crepitus in both knees (suggestive of osteoarthritis). Blood examination revealed high eosinophil (a type of white blood cell) count and raised ESR. Other laboratory investigations were normal. Fever and myalgia responded to steroids and painkillers. The patient went back to Nigeria after 3 weeks or so. Eosinophilia Myalgia syndrome is closely linked to ingestion of tryptophan in diet although evidence of its ingestion is not essential for diagnosis of this disease. Tryptophan was, therefore, withdrawn from US market in 1991 but sales were again allowed from 2001. Tryptophan is available in food stores as diet supplement. People use it for insomnia, depression and menstrual problems. Average daily dose of 1250 mg for 6 months to 9 years is supposed to lead to this disease. Tryptophan is a routine constituent of most protein-based foods or dietary proteins. Chocolates, oats, bananas, mangoes, dried dates, milk and milk products, spirulina, peanuts, red meat, eggs, fish, poultry and turkey are all rich sources of tryptophan. Symptoms of Eosinophilia Myalgia syndrome can be difficult to respond to therapy. Muscle pain and weakness, fatigue, joint pains, breathlessness, memory loss and numbness can persist even at the end of 1-4 years.
A good history and detailed clinical examination of patient are extremely important for proper diagnosis of over 100 types of arthritis. Recognition of patterns of joint involvement (topography) as well as those of disease presentation and progression is essential for correct clinical diagnosis. In rheumatology practice, a working diagnosis can usually be made on proper examination of the patient. Laboratory tests including X-Rays are ordered later for confirmation of diagnosis, ruling out other possible causes, estimating level of disease activity or monitoring drug toxicity. As with any other investigations, these must be obtained from a reliable laboratory and the results should always be interpreted in view of clinical picture. These tests are costly and must not be used indiscriminately. Laboratory studies are useful in arthritis only if ordered in an appropriate clinical situation and interpreted accordingly. Measurement errors, laboratory variations due to various factors and inherent limitations must always be born in mind. A positive test in absence of appropriate clinical setting can generally be overlooked.
Pain is a universal phenomenon. It is an unpleasant sensation felt by more than half of the world's population. Pain is a perception which is real and leads to considerable deterioration of quality of life in patients with arthritis and other rheumatological conditions. It has complex causes and is a leading cause of morbidity. Pain limits ability to perform day-to-day activities, maintain social relationships and lead productive life. 'Pain is a perfect misery, the worst of evils, and when excessive, overturns all patience' (John Milton). Pain as a sensation starts from sensors in skin and other organs and reaches brain via nerve channels passing through spinal cord. It can be nociceptive (produced by injury), neuropathic (due to irritation of nerve), mixed or psychological. Fast pain is one which occurs after an injury. Localization of this pain is sharp and accurate and is protective in nature. Slow pain is a delayed perception after tissue injury that helps in healing. Descending chemical and electrical impulses from brain modulate pain perception to a significant extent. Pain may be described in various ways such as sharp, shooting, burning, nagging, dull and aching. Being a subjective sensation, it is very difficult to quantify pain. Severity of pain is generally measured by visual analog or numerical rating scales which ask the patients to rate the severity of their pain on a 1-10 or 1-100 scale. Back pain can be as severe as cancer pain whereas severity of arthritis pain can be almost half that of pain during childbirth. Pain leads to restlessness, anxiety and depression. Physical effects of pain include nausea, vomiting, palpitations, urinary incontinence, rise in blood pressure, etc. Pain does need treatment but it must be realized that pain is a protective phenomenon. Pain in arthritis limits movements that can be damaging. Chemical substances released during slow pain help in healing. One must learn to bear and live with at least some of arthritis pain. We have many effective drugs for pain relief, but not all work in patients in identical way. Though invaluable in pain management, they are notorious for causing skin rashes, acidity and other more severe abdominal problems, liver and kidney toxicity as well as effects on heart and blood pressure. They interact with some other drugs such as those used for diabetes and blood pressure. Control of disease causing pain e.g. rheumatoid arthritis alleviates need for pain medication.
Guidelines by European League against Rheumatism (EULAR) on use of pain killers include following:
1. Avoid long term use
2. Use as and when required and not continuously
3. Use lowest effective dose for shortest duration
4. Use only one painkiller at a time
5. Avoid in stomach ulcer and kidney disease.
Prescription of painkillers must be individualized after assessment of need and risk factors. Paracetamol (maximum dose: 4 grams/day) is a comparatively safe painkiller. Local application of heat or ice pack or an ointment should also be tried in all cases of musculoskeletal pain. Patient education regarding self-help, social support, joint protection and assistive devices, physical therapy and exercise, acupuncture and music therapy are important non-drug measures in pain management.
As per World Health Organization (WHO) criteria, your BMI should fall between 18.5 and 24.9 to be normal. If your BMI is between 25 and 29.9 you are overweight. A BMI ≥ 30 classifies you as obese. People who have a BMI of ≥ 40 fall into the ‘morbidly obese’ weight bracket.
Diet and do-don'ts (pathya - suitable versus harmful diet and lifestyle) have gained importance in our country since the period of Ramayan and Mahabharat. Food keeps alive our journey of life hence it is not unnatural for people to think that there is a relation between diet and disease. The importance of pathya is rooted deep in the minds of people over hundreds of years. Scientists all over world are looking for co-relation between diet and arthritis for over last seven decades. Although over half of the arthritis patients are following some or the other pathya, there is no sufficient evidence for some particular diet or dietetic item triggering or flaring or curing arthritis. Magic cure is certainly impossible with the help of diet therapy.
Diet and food supplements are advertised in various books, periodicals and on internet. There is no scientific proof in favor of diet supplements which are usually expensive. Patients fall prey to these advertisements which are usually more expensive than the actual disease modifying drugs. Companies rob these patients by paying hefty commission to their selling agents. Inflammatory arthritis, by its very nature, is a disease of relapse and remissions. Remission in a particular patient on starting with a particular therapy is advertised as success of that particular therapy. Poor people have no knowledge of checking the validity of tall claims in the advertisement.
The list of pathya is sometimes so long that there remains nothing to eat. Some practitioners advise fasting which is not advocated even in Ayurveda. Vagbhata says that insufficient diet reduces strength, nourishment as well as luster and causes all vata-diseases ( Sutra sthan 8/3). Some people advise liquid diet only. These measures may reduce pain to some extent but are not effective in shortening the duration of morning stiffness or controlling the disease or in improving the functional status. Patients start feeling better after 4-5 days of fasting. Fasting can lead to severe fatigue, weakness and weight loss. Switching back to regular diet brings the disease to original status once again. Fasting, liquid diet or other pathya is difficult to maintain indefinitely. Such diets have an overt risk of malnutrition.
It must be understood that arthritis is of more than 100 types which are classified into two major classes-degenerative and inflammatory. It obviously means that the pathya in these two classes of arthritis is not the same because of an altogether different disease process. It is usually advisable to change the diet step by step. One should identify a few dietary items that increase the pain or stiffness. Once identified, such items may be avoided for a month or so. Reappearance of symptoms on reintroduction of suspected item indicates a sort of allergy. Such food items should never ever be consumed again.
Many rheumatologic diseases affect young women of childbearing age. Pregnancy alters immune status and is always a cause of concern in this age group. Effective use of better drugs and rigorous monitoring can now lead to remission of disease activity in many cases. Safe pregnancy and healthy child are thus possible in most cases with controlled disease activity. This issue must be carefully discussed before planning pregnancy in every patient desirous of child bearing. Pregnancy in rheumatic diseases requires a multidisciplinary coordinated approach for best possible outcome.
Pregnancy related issues of some important rheumatologic diseases are listed below:
Rheumatoid Arthritis (RA) : A lower birthrate in patients with RA is possibly due to choices of patients to limit family size rather than effect of the disease on fertility. Disease activity decreases during pregnancy in 75-95% patients. The improvement starts in first trimester and continues till delivery. There is no evidence of fetal growth retardation or increased incidence of abortions. No special monitoring is required during pregnancy. Drugs such as methotrexate and leflunomide must be discontinued 2 and 24 month respectively before planning pregnancy. Pain control during pregnancy with RA should be achieved with safe drugs and non-pharmacologic measures (rest, splints, fomentation, icepack, etc). RA is known to flare up after delivery. New onset of RA following delivery is also common. Use of routine anti-rheumatic drugs is possible after delivery with properly timed breast feeding.
Systemic Lupus Erythematosus (SLE) :Patients with SLE appear to be less fertile due to disease effect (irregular or no menses) or due to effect of drugs (glucocorticoids and cyclophosphamide). Patients on cyclophosphamide are less likely to develop infertility (failure of ovaries) if cyclophosphamide is started at a younger age ( More then 26 years). Ovarian failure is more likely with higher cumulative dose. Concurrent use of Gonadotropin Releasing Hormone reduces the risk of premature ovarian failure. SLE patients are more likely to develop flares during pregnancy (unproven observation) which are usually mild and respond to standard therapy. Patients with inactive disease are less likely to develop flares. Pregnancy, therefore, should be planned during quiescent disease. Risk of intrauterine growth retardation, abortions and stillbirth is generally higher in SLE patients. Antibodies are transmitted to fetus during weeks 16-32 of gestation and can be harmful to fetus. Careful monitoring after week 16 is, therefore, advisable. These antibodies are usually destroyed with first 6 months of life.
Ankylosing spondylitis and other spondyloarthropathies : Pregnancy improves peripheral arthritis and eye problems but worsens back pain. Increase in back pain is possibly due to mechanical causes.
Management of chronic diseases demands informed and active participation of patient. An intelligent and educated patient with some faith in a selected medical specialist is usually better placed for good therapeutic outcome. An intelligent patient can easily analyze own symptoms and express them to doctor. Patients must provide true and correct information to their doctor. Anxious, depressed, forgetful, timid or violent patients with chronic physical disease are usually difficult to treat. Therapy is likely to be unsuccessful in patients who keep on experimenting with dosages of their prescribed drugs. They must follow prescribed treatment religiously and inform new developments correctly. Trust in physician increases chances of adherence to treatment plan. A good doctor-patient relationship can only be built upon trust. Patients must also understand and accept limitations of present therapy in chronically damaged joints and other organs and define expectations accordingly. Finally, adequate resources to fund cost of therapy are absolutely essential.
Washing your hands with soap and water or using alcohol-based hand rub kills viruses that may be on your hands.
When someone coughs or sneezes they spray small liquid droplets from their nose or mouth which may contain virus. If you are too close, you can breathe in the droplets, including the COVID-19 virus if the person coughing has the disease.
Hands touch many surfaces and can pick up viruses. Once contaminated, hands can transfer the virus to your eyes, nose or mouth. From there, the virus can enter your body and can make you sick.
Make sure you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. Then dispose of the used tissue immediately.
The most common symptoms of COVID-19 are fever, tiredness, and dry cough. Some patients may have aches and pains, nasal congestion, runny nose, sore throat or diarrhea. These symptoms are usually mild and begin gradually. Some people become infected but don’t develop any symptoms and don't feel unwell. Most people (about 80%) recover from the disease without needing special treatment. Around 1 out of every 6 people who gets COVID-19 becomes seriously ill and develops difficulty breathing. Older people, and those with underlying medical problems like high blood pressure, heart problems or diabetes, are more likely to develop serious illness. People with fever, cough and difficulty breathing should seek medical attention.
There is no specific medicine to prevent or treat coronavirus disease (COVID-19). People may need supportive care to help them breathe.
If you have mild symptoms, stay at home until you’ve recovered. You can relieve your symptoms if you:
- - Rest and Sleep
- - Weep Warm
- - Drink Plenty of Liquids
- - Use a room humidifier or take a hot shower to help ease a Sore Throat and Cough
If you develop a fever, cough, and have difficulty breathing, promptly seek medical care. Call in advance and tell your health provider of any recent travel or recent contact with travelers.
The following measures ARE NOT effective against COVID-2019 and can be harmful:
- - Smoking
- - Wearing multiple masks
In any case, if you have fever, cough and difficulty breathing seek medical care early to reduce the risk of developing a more severe infection and be sure to share your recent travel history with your health care provider.
Currently, the source of SARS-CoV-2, the coronavirus (CoV) causing COVID-19 is unknown. All available evidence suggests that SARS-CoV-2 has a natural animal origin and is not a constructed virus. SARS-CoV-2 virus most probably has its ecological reservoir in bats. SARS-CoV-2, belongs to a group of genetically related viruses, which also include SARS-CoV and a number of other CoVs isolated from bats populations. MERS-CoV also belongs to this group, but is less closely related.
The virus that causes COVID-19 is mainly transmitted through droplets generated when an infected person coughs, sneezes, or speaks. These droplets are too heavy to hang in the air. They quickly fall on floors or surfaces.
You can be infected by breathing in the virus if you are within 1 metre of a person who has COVID-19, or by touching a contaminated surface and then touching your eyes, nose or mouth before washing your hands.

